Accurate completion of the CMS 1500 form is paramount for timely reimbursement, especially for specialized services like ambulance transport. This comprehensive guide focuses on the critical fields for ambulance billing: Boxes 24e (Diagnosis Pointer), 24f (Charges), and 24g (Days or Units). Understanding these sections is key to preventing claim denials and ensuring proper payment for your services.
Essential Fields for Ambulance Billing on the CMS 1500
Below is a detailed breakdown of how to correctly fill out Boxes 24e, 24f, and 24g specifically for ambulance services.
| Block No. | Block Name | Block Code | Detailed Instructions for Ambulance Billing |
| 24e | Diagnosis Pointer | M | This block is used to link each service line to the specific diagnosis (from Box 21) that justifies the service. You may enter up to four digits (1, 2, 3, or 4). If the ambulance service was provided for the primary diagnosis in Block 21, enter 1. For a secondary diagnosis, enter 2, and so on. This is critical for demonstrating medical necessity for CMS 1500 diagnosis pointer 24e ambulance claims. Scenarios for Ambulance Services:
|
| 24f | $Charges | M | Enter your usual charge to the general public for the service(s) provided. This is your standard, non-negotiated price for a given service, consistent for all patients regardless of payer. Do not include a decimal; implicitly, the last two digits represent cents. For example, if your usual charge is sixty-five dollars ($65.00), enter 6500. When calculating charges for CMS 1500 box 24f for multiple units of service (e.g., mileage), multiply your usual per-unit charge by the number of units billed and enter the total amount. Examples for Ambulance Services:
Maintaining a clear fee schedule and applying it consistently is crucial for compliance. |
| 24g | Days or Units | M | This field indicates the number of units, services, or items provided. For ambulance services, this primarily refers to either a single unit for the base rate (e.g., A0428, A0429) or the number of billable miles for mileage (A0425). Understanding how to report units on CMS 1500 box 24g for ambulance and specific CMS 1500 mileage billing guidelines is vital. Billing for Ambulance Mileage (HCPCS A0425): Medicare typically reimburses for loaded miles, meaning miles traveled with the patient onboard. Billable mileage is paid beyond the first 20 loaded miles of a single ambulance transport. This ‘first 20 miles’ acts as a non-reimbursable threshold, not a deductible that applies to each leg of a round trip or cumulative transports. To calculate billable units for A0425:
Examples for Mileage Calculation:
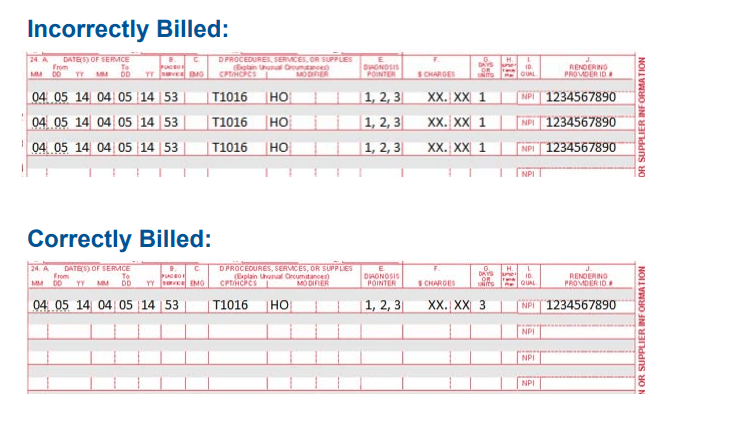
Multiple Transports, Same Date/Recipient/Code: If a recipient has more than one ambulance transportation episode on the same date of service that requires the same Procedure Code/Modifier combination, the episodes should be “mulled” (combined) on a single claim line. In Box 24G (Units), indicate the total number of billable units across all such episodes. For example, if two separate transports each generated 15 billable miles (after deducting 20 miles from each transport individually), the claim line would show a total of 30 units. It is crucial to meticulously document in the recipient’s file the reason why it was necessary to bill for more than 1 unit, especially for mileage or multiple base rate services on the same day if applicable and justified. |
Common Errors and Best Practices in Ambulance Billing (Boxes 24e, 24f, 24g)
Avoiding common mistakes in these critical fields can significantly reduce claim denials and improve revenue cycle management for ambulance services.
- Diagnosis Pointer (24e) Errors:
- Mismatched Pointers: Linking a service to an irrelevant diagnosis, or failing to update pointers when the primary reason for transport changes.
- Missing Pointers: Omitting the pointer altogether, leading to questions about medical necessity.
Best Practice: Always ensure the diagnosis pointer accurately reflects the primary medical necessity for each specific service on that line.
- Charges (24f) Errors:
- Inconsistent Usual Charges: Varying charges for the same service to different payers or patients without proper justification.
- Incorrect Calculation for Multiple Units: Failing to multiply the per-unit charge by the correct number of units (e.g., for mileage).
Best Practice: Maintain a transparent and consistently applied fee schedule. Regularly review and update charges to reflect fair market value while adhering to “usual and customary” guidelines.
- Days or Units (24g) Errors:
- Mileage Calculation Mistakes: Incorrectly deducting the 20-mile threshold, billing for unloaded miles when not covered, or miscalculating total loaded miles.
- Multiple Transport Misreporting: Not combining units for same-day, same-code transports, or incorrectly combining them.
Best Practice: Implement robust internal audit processes for mileage logs and unit calculations. Provide ongoing training to billing staff on complex rules like the “first 20 miles” for A0425 and “mulled” claim lines.
Thorough documentation in the patient care report (PCR) is the foundation for accurate billing in all these fields.
Official CMS Reference for Ambulance Billing
For the most authoritative guidance on ambulance services and CMS 1500 form completion, refer to the official Medicare Claims Processing Manual. Specifically, Chapter 15 provides detailed information on ambulance services:
Medicare Claims Processing Manual, Chapter 15 – Ambulance Services (PDF)
Please remember to bill same services on one line item with the corresponding number of units where appropriate, especially for combined mileage units.
Source