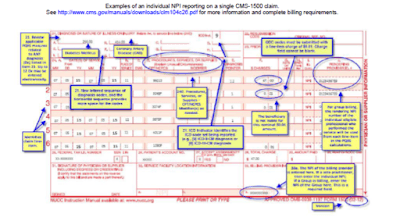
PQRS SAMPLE CMS 1500 CLAIM submission
The patient was seen for an office visit (99213). The provider is reporting several measures related to diabetes, coronary artery disease (CAD), and urinary incontinence:
Measure #2 (LDL-C) with QDC 3048F + diabetes line-item diagnosis (24E points to DX 250.00 in Item 21);
Measure #3 (BP in Diabetes) with QDCs 3074F + 3078F + diabetes line-item diagnosis (24E points to Dx 250.00 in Item 21);
Measure #6 (CAD) with QDC 4011F + CAD line-item diagnosis (24E points to Dx 414.00 in Item 21); and
Measure #48 (Assessment – Urinary Incontinence) with QDC 1090F. For PQRS, there is no specific diagnosis associated with this measure. Point to the appropriate diagnosis for the encounter.
Note: All diagnoses listed in Item 21 will be used for PQRS analysis. Measures that require the reporting of two or more diagnoses on claim will be analyzed as submitted in Item 21.
NPI placement: Item 24J must contain the NPI of the individual provider that rendered the service when a group is billing.
If billing software limits the line items on a claim, you may add a nominal line-item charge of a penny to one of the QDC line items on that second claim. PQRS analysis will subsequently join both claims based on the same beneficiary, for the same date-of-service, for the same TIN/NPI and analyze as one claim.
The patient was seen for an office visit (99213). The provider is reporting several measures related to diabetes, coronary artery disease (CAD), and urinary incontinence:
Measure #2 (LDL-C) with QDC 3048F + diabetes line-item diagnosis (24E points to DX 250.00 in Item 21);
Measure #3 (BP in Diabetes) with QDCs 3074F + 3078F + diabetes line-item diagnosis (24E points to Dx 250.00 in Item 21);
Measure #6 (CAD) with QDC 4011F + CAD line-item diagnosis (24E points to Dx 414.00 in Item 21); and
Measure #48 (Assessment – Urinary Incontinence) with QDC 1090F. For PQRS, there is no specific diagnosis associated with this measure. Point to the appropriate diagnosis for the encounter.
Note: All diagnoses listed in Item 21 will be used for PQRS analysis. Measures that require the reporting of two or more diagnoses on claim will be analyzed as submitted in Item 21.
NPI placement: Item 24J must contain the NPI of the individual provider that rendered the service when a group is billing.
If billing software limits the line items on a claim, you may add a nominal line-item charge of a penny to one of the QDC line items on that second claim. PQRS analysis will subsequently join both claims based on the same beneficiary, for the same date-of-service, for the same TIN/NPI and analyze as one claim.